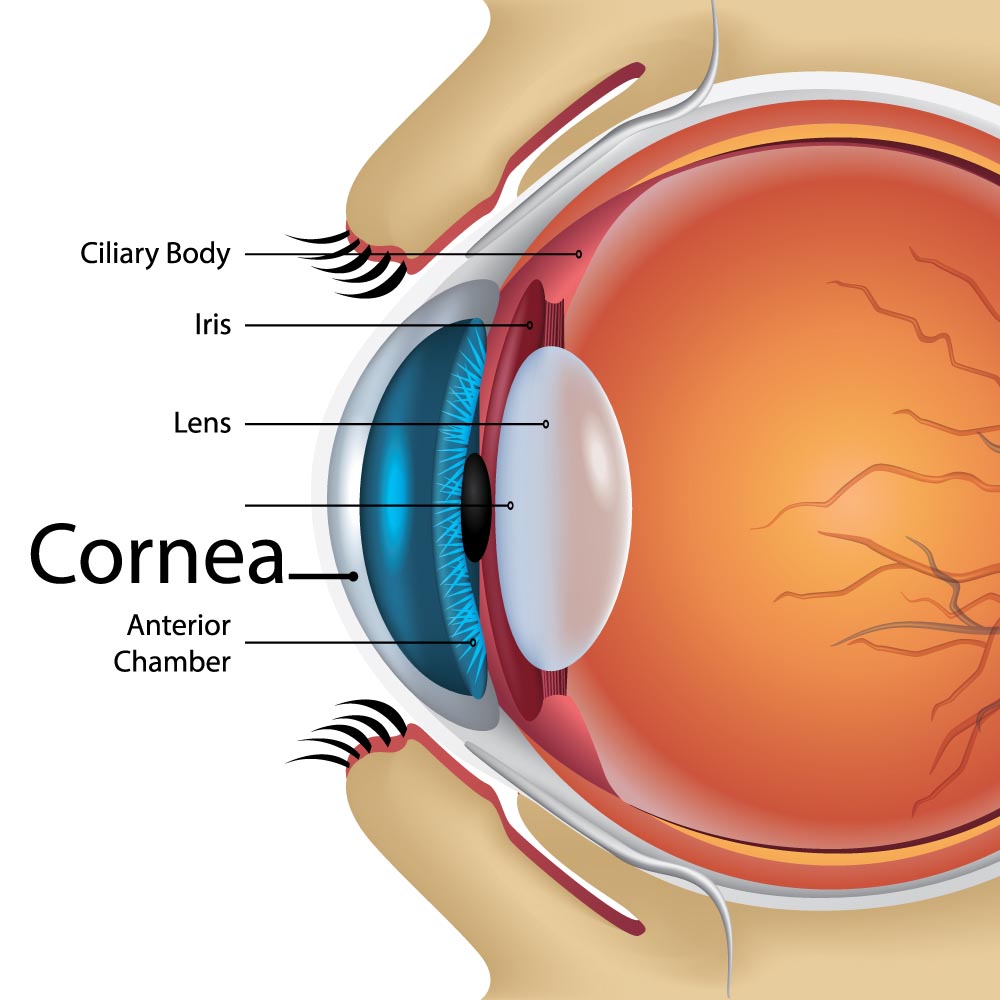
Cornea
The Cornea is the eye’s window.
Cornea’s integrity is of vital importance in order for us to see clearly. Eye diseases and injuries may affect the cornea. The most common problems affecting the cornea are:
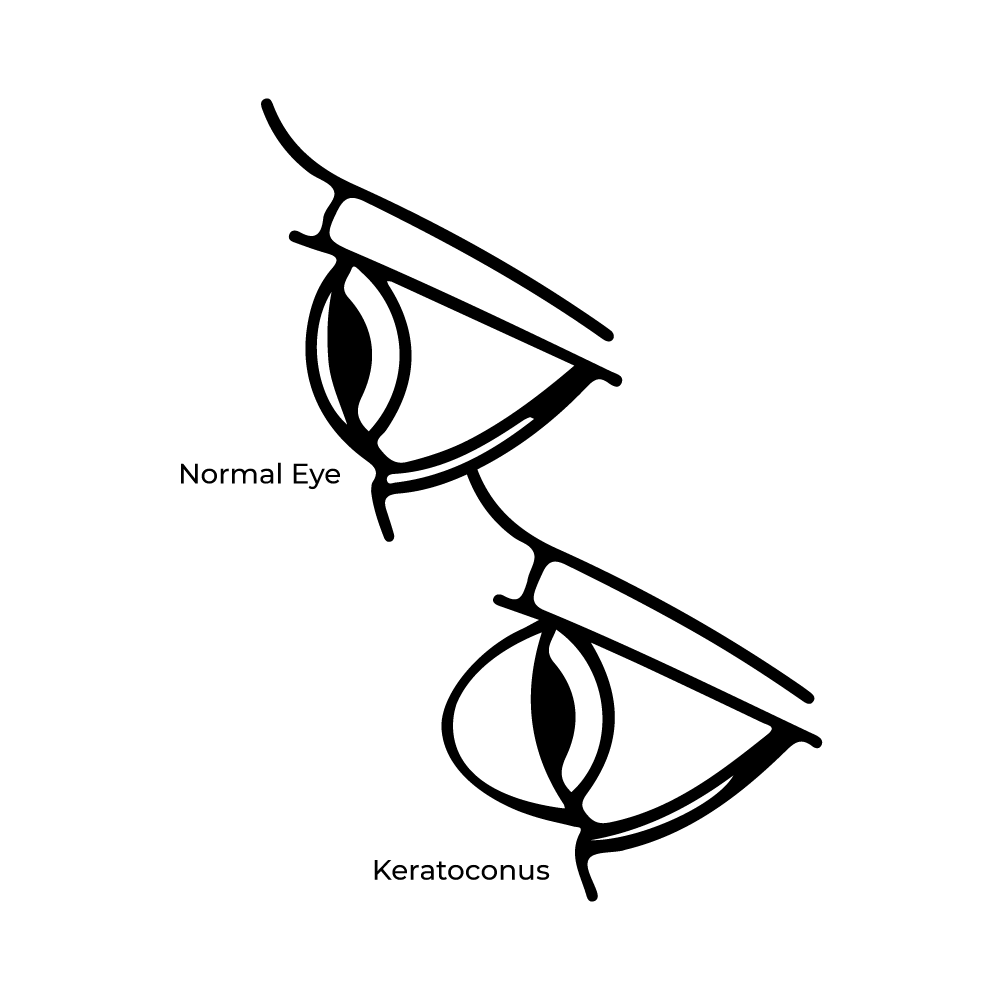
- Keratoconus, where the cornea adopts the shape of a cone causing high levels of astigmatism.
- Fuch’s dystrophy, where the inner lining of corneal cells stop working.
- Trauma and Infections caused by contact lens wear
- Previous eye surgeries.
How are corneal diseases treated?
Many corneal conditions can be treated medically with eye drops or simple observation. When the condition cannot be treated medically, and visual acuity is sub-optimal, then we can consider using lasers (Phototherapeutic Keratectomy) or surgeries such as corneal transplants to correct the problem. Full thickness (peneterating keratoplasty) or partial thickness transplants (DSEK/DMEK) are performed depending on the type of corneal disease present. Our corneal surgeon at Castle Hills Eye Specialists will perform a detailed corneal examination and determine what the best treatment option for you is.
Keratoconus (KC)
What Causes Keratoconus?
No one knows what causes keratoconus, although genetic and environmental factors are thought to be involved. Around 1 in 10 people with keratoconus also have a parent with the condition. If you have family history of keratoconus, get your child eyes checked and monitored because the sooner KC is diagnosed and treated, the less vision they will lose.
What are the Risk Factors for KC?
- Having a family history of keratoconus
- Rubbing your eyes vigorously
- Having certain conditions, such as Down syndrome, Ehlers-Danlos syndrome, retinitis pigmentosa, hay fever and asthma
- Chronic eye inflammation from allergies or irritants
- Age. Keratoconus is often discovered in the teenage years
What are the symptoms?
- Constantly and regularly changing glasses
- Blurry vision
- Increased light sensitivity
- Difficulty driving at night
- A halo around lights and ghosting (specially at night)
- Eye strain
- Headaches and eye pain
- Eye irritation, excessive eye rubbing
How is KC diagnosed?
Keratoconus can be diagnosed through a routine eye exam. Your ophthalmologist will examine your cornea, and may measure its curvature. This helps show if there is a change in its shape. Your ophthalmologist may also map your cornea’s surface using a special computer. This detailed image shows the condition of the cornea’s surface.
What is the treatment for Keratoconus?
Mild Keratoconus
Glasses or Contact lenses. Your vision can be corrected with eyeglasses or disposable/reusable contact lenses. As keratoconus progresses, the cornea becomes more irregularly shaped. Eye glasses and soft contact lenses can not correct for the irregular corneal shape.
Moderate Keratoconus
Rigid Gas Permeable Lenses. RGP lenses can be custom designed for the unique shape of the KC cornea and are easy to apply, remove, and care for. These lenses provide good vision correction, but some patients are unable to tolerate their wear over long periods of time.
Intacs. This is a small curved device that your ophthalmologist surgically puts in your cornea to help flatten the curvature of your cornea to improve vision. The primary goal of Intacs in keratoconus is to improve contact lens fitting, comfort, vision and to avoid corneal transplantation.
Intacs can also be used after other keratoconus procedures, such as cross-linking. If necessary, Intacs can be safely removed and the cornea will generally return to its preoperative condition
Collagen cross-linking (CXL). Is a minimally invasive outpatient procedure, FDA approved that combines the use of ultra-violet light with riboflavin drug drops to create new collagen bridges which lead to the stiffening of the cornea, to slow or prevent further progression of the condition and preserve your vision.
Severe Keratoconus
Corneal transplant. When symptoms are severe, a corneal transplant may be needed due to scarring, extreme thinning or contact lens intolerance. This is a surgical procedure that replaces the keratoconus cornea with healthy donor tissue.
The overall success rate of a corneal transplant is very high using modern eye-banking and surgical techniques. However, there are many factors that influence the outcome. For instance, keratoconus has one of the best prognoses for good vision with a greater than 90% chance of a clear graft.
With subspecialty fellowship training in corneal surgery and years of experience working with patients with Keratoconus, Dr. Sepulveda will give you the best possible treatment options for your particular case.
